Over time, doctors learned that traditional over-the-counter medications like non-steroidal anti-inflammatories did very little to ease the symptoms of peripheral neuropathy. While prescription nerve pain medications like Gabapentin worked better, the overall success rate of this type of medication was also low. For some time, opioids were the “most successful” alternative. But, as we mentioned, the high risk of addiction and overdose doesn’t make this a very solid option. It certainly isn’t one that many doctors want to explore for their patients. As the area of pain management has continued to evolve and advance, science has explored the benefits of high-frequency spinal cord stimulation. This modality is not new. It’s been around for more than 15 years and has been used thousands of times to treat nerve injuries and spinal pain caused by trauma. Most recently, we’ve begun to successfully utilize spinal cord stimulation for patients with peripheral diabetic neuropathy.
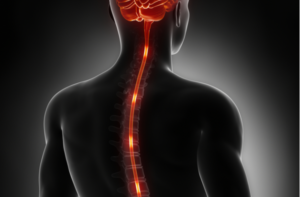
What is Spinal Cord Stimulation?
For many years, cardiologists have used pacemakers to help a specific set of patients. Spinal cord stimulation is like a pacemaker for the spinal cord. One of the best things about his modality is that it is very commonly used on a trial basis. Patients commit to maybe a week of treatment rather than their entire lifetime, which significantly decreases the risk associated with treatment. A spinal cord stimulation trial involves the implantation of thin wires attached to electrodes. The electrical pulses that stimulate the spinal cord are delivered from an external device that is attached to the electrodes (also external). In this way, the patient essentially “test drives” the treatment. At the end of the trial period, the doctor removes the temporary devices and discusses the difference that was experienced, if any. If the spinal cord stimulation was successful at significantly reducing symptoms, the patient can choose to have a permanent device implanted.
Spinal cord stimulation works by delivering a gentle electrical current to the spinal cord. The implantation procedure usually requires no more than about 90 minutes. In one of the most comprehensive studies on this modality, researchers found that 80 to 90 percent of participants achieved lasting pain relief. Over a period of two years, the study found that participants reported better sleep, higher quality of life, and, yes, less pain. The results of studies on spinal cord stimulation led to the FDA clearance of this modality as a treatment option for peripheral diabetic neuropathy.
At the first indication of symptoms of peripheral diabetic retinopathy, patients stand a good chance of management using medication and lifestyle habits to reduce blood sugar levels. When this condition has been present for some time, it needs a different approach. To learn more about our Spinal Cord Stimulator Trial, contact Nova Interventional Pain & Spine at 571-510-3815.